When is hysteroscopy needed?
The most common indications for hysteroscopy include:
- Investigation of the causes of abnormal vaginal bleeding
- Lysis of adhesions, which usually result from infections or previous surgeries in the area
- Removal of endometrial polyps
- Removal of fibromyomas in the endometrial cavity (submucosal fibromyomas)
- Endometrial biopsy
- Investigation of causes of infertility or repeated miscarriages
How is hysteroscopy performed?
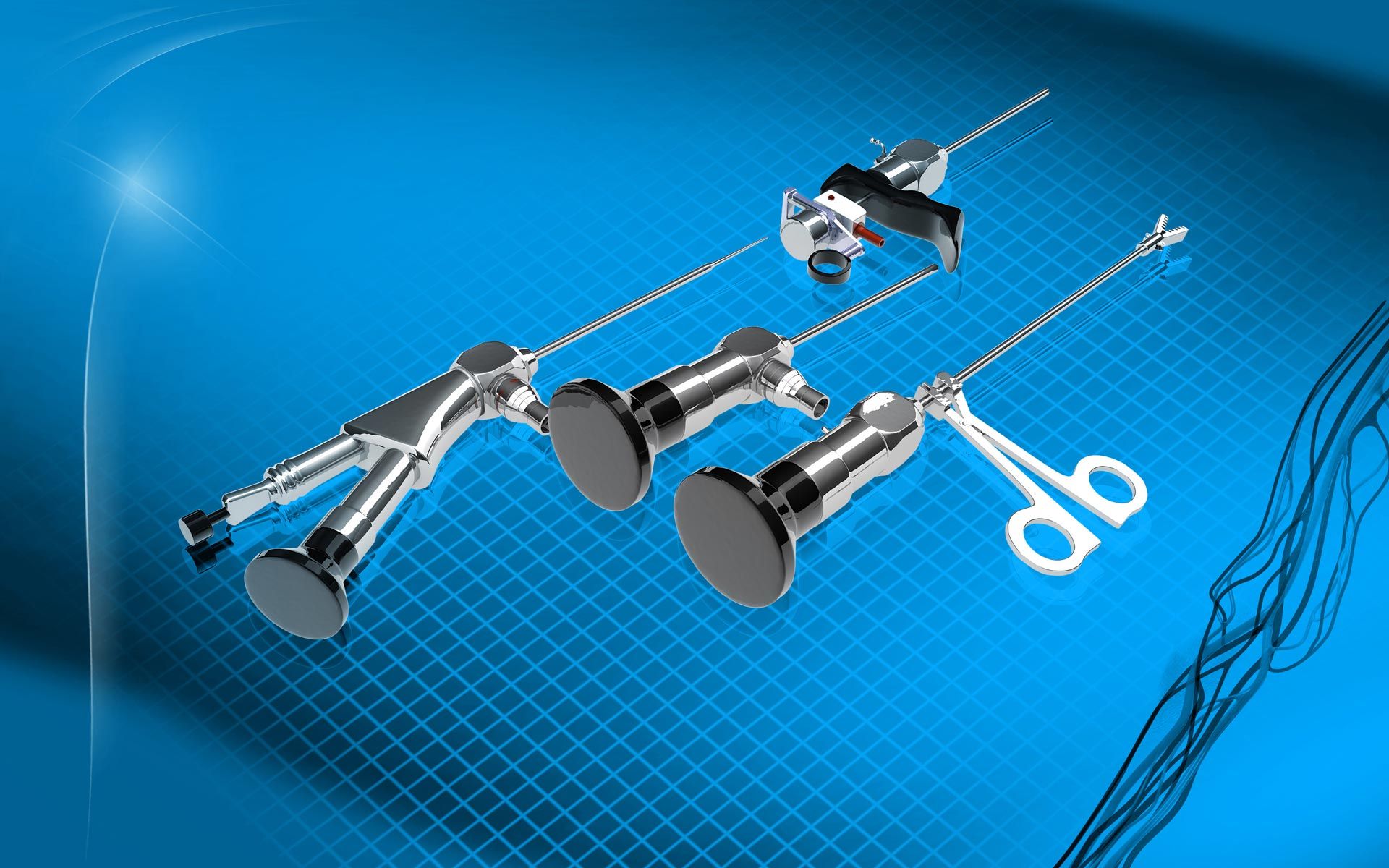
Hysteroscopy should be planned when the patient is not menstruating, ideally before ovulation (1st phase of menstrual cycle). The type of anaesthesia (e.g., sedation, general or local anaesthesia) is selected based on the time requirements of the surgery. To insert the hysteroscope in the endometrium more easily, dilation of cervical tube might be necessary. This can be performed through the administration of intravaginal medication before the surgery or/and the use of special dilators during the surgery. Moreover, to ensure the best visibility possible, the gynaecologist dilates the endometrial cavity intraoperatively with a special fluid (e.g., normal serum, Ringer's lactate solution), the quantity of which is carefully documented. The doctor simultaneously pushes the hysteroscope inside and carefully examines the endometrial surface and the entrance to the fallopian tubes to see if there is any kind of pathology. If the findings of hysteroscopy require so, special tools are placed in the endometrial cavity through the hysteroscope to perform the surgery (e.g., biopsy, removal of an endometrial polyp, etc.).
What should the patient expect after hysteroscopy?
After surgery, the patient will need to stay in the hospital for some time, especially if she has undergone general anaesthesia or an invasive procedure (e.g., removal of an endometrial polyp). Shortly thereafter, she might complain about mild menstrual pain, which can be fully managed with typical pain relief medication, or slight vaginal bleeding. She can return to her daily activities almost immediately, while sexual contact is usually allowed two weeks later. In the very rare case that she experiences fever, foul-smelling discharge, heavy vaginal bleeding or intense pain in the lower abdomen, the patient should contact her doctor immediately.