General information
Endometrial cancer is the most common malignancy of the female genital system in developed countries. It occurs in the endometrium, i.e., in the tissue that covers the uterine cavity, mainly after menopause. In most cases it is diagnosed at an early stage, so the cure rates are very high.
What are the main symptoms of endometrial cancer?
The symptoms of endometrial cancer include:
- Abnormal vaginal bleeding. Before menopause, the increased amount of period blood, longer periods and vaginal bleeding between periods need further investigation, especially if there are coexisting risk factors for endometrial cancer. After menopause, any episode of vaginal bleeding is an indication for immediate gynecological examination.
- In rarer cases, unusual vaginal fluids, pain or feeling of pressure in the pelvic area, weight loss and prolonged weakness may be signs of endometrial cancer.
What are the risk factors for developing endometrial cancer?
The risk factors for developing endometrial cancer include:
- Age >50 years
- Obesity
- Taking estrogens as a hormone replacement therapy during menopause, when not accompanied by progesterone
- Nulliparity
- Hypertension and diabetes
- Anovulatory cycles (periods at sparse intervals throughout the year), such as in polycystic ovary syndrome (PCOS)
- Intake of tamoxifen, which is used to treat breast cancer, especially when taken by older women for many years
- Positive family history of endometrial, colon or ovarian cancer (Lynch syndrome)
It is noted that the presence of one or more risk factors in a woman does not necessarily mean that she will develop endometrial cancer. However, it is advisable to consult her doctor.
How can a woman reduce the risk of developing endometrial cancer?
Unfortunately, there is no way to provide complete protection against endometrial cancer. However, the following may reduce the risk of developing the disease:
- Using birth control pills
- Maintaining a normal body weight and increased physical activity
- Taking progesterone and estrogens, as part of a postmenopausal hormone replacement therapy
In case of hereditary predisposition (Lynch syndrome).
Are there any screening tests for endometrial cancer?
In asymptomatic women without particular risk factors, there is no standard way to prevent endometrial cancer. Unlike cervical cancer, the PAP test CANNOT reliably diagnose precancerous lesions or endometrial cancer. Therefore, women should be aware of the main symptoms of the disease. If they notice any of the above signs or run high risk for endometrial cancer (e.g., they have a hereditary predisposition), they should immediately contact their doctor for further consultation and treatment.
How is endometrial cancer diagnosed?
The initial evaluation of the patient with suspicious symptoms of endometrial hyperplasia (e.g., abnormal vaginal bleeding) includes genital ultrasound. Depending on the findings and her general history, the doctor may recommend an endometrial biopsy, usually with a diagnostic abrasion. In some cases, hysteroscopy is recommended before diagnostic abrasion. In this way, under direct vision, it is possible to identify very small areas inside the endometrial cavity with suspicious features, thus take more targeted biopsies.
What information is expected from the endometrial biopsy?
If there is endometrial cancer, the biopsy will give us information about the histological type and the tumor differentiation (grade). The most common histological type is the endometrial. The rarest and more aggressive histological types are serous, clear cell “sugar” tumor, undifferentiated and carcinosarcoma. The grade of tumor differentiation is related to its biological behavior and is divided into grades 1, 2 and 3, with the latter being considered a high risk.
What should I do if I am diagnosed with endometrial cancer?
If the endometrial biopsy shows cancer, the next step for the patient is to visit a Gynecologic Oncologist, i.e. a Gynecologist with official individualization in treating gynecologic cancers. The Gynecologic Oncologist has all the necessary knowledge and technical skills to evaluate the patient, to provide the appropriate surgical treatment and to coordinate the rest of the treatment (if necessary) and the subsequent monitoring of the patient.
Surgical treatment
Endometrial cancer is treated surgically. The information we get from the histological examination of the surgical products determines the stage of the disease (i.e. its extent) and the need for additional treatment.
For the best schedule of the surgery, the imaging of the patient preoperatively, usually with magnetic resonance imaging (MRI) of the lower abdomen with intravenous contrast is useful. However, depending on the histological type and the grade of differentiation of the tumor at the initial endometrial biopsy, additional examinations may be required, such as a CT scan of chest and upper-lower abdomen with intravenous and oral contrast. The use of cancer markers (CA-125) is of limited value in most patients with endometrial cancer.
What does an endometrial cancer surgery include?
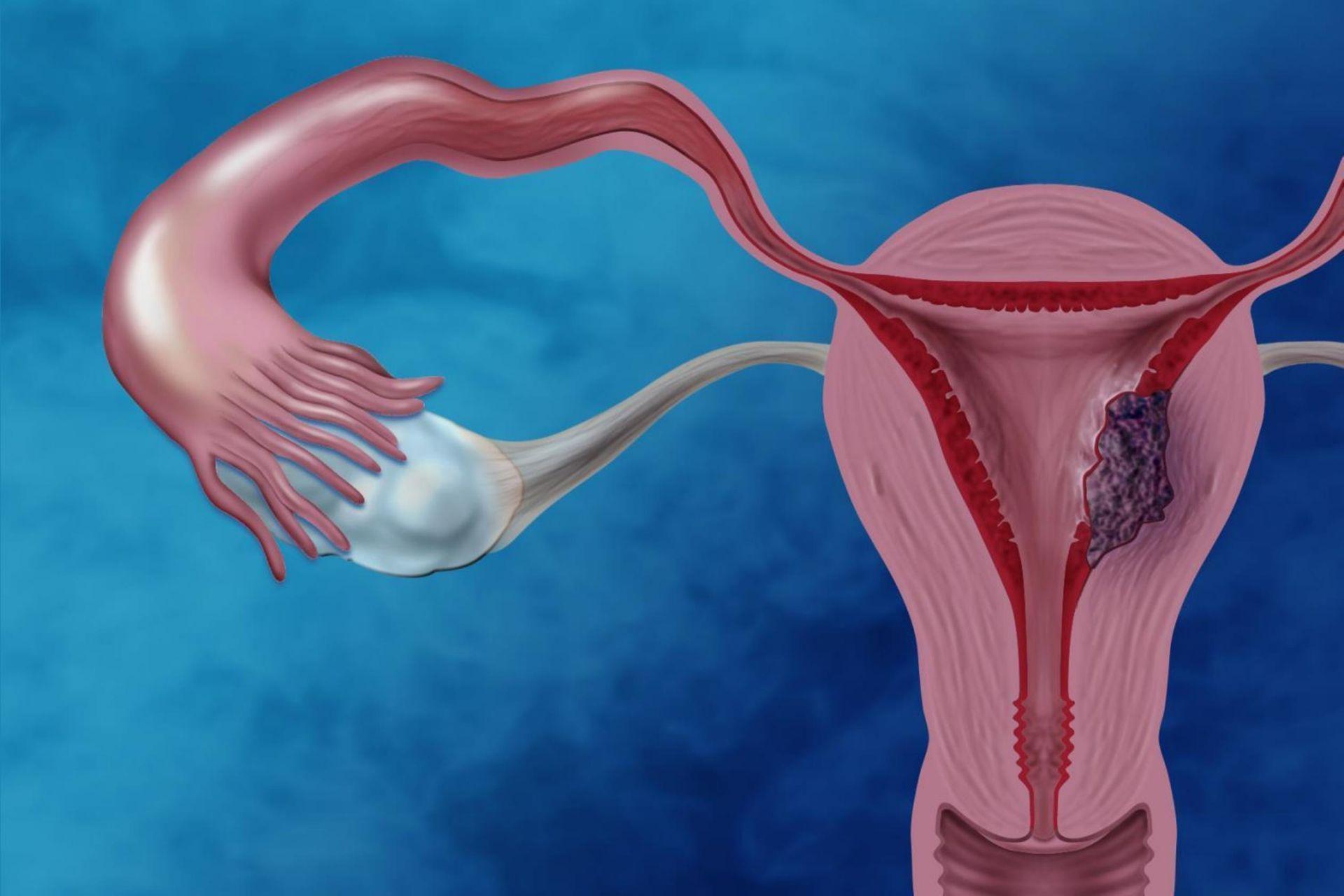
The important part of endometrial cancer surgery is the removal of the uterus (total hysterectomy) and its appendages (fallopian tubes, ovaries).
More specifically:
- When entering the peritoneal cavity, the Gynecologic Oncologist carefully examines the peritoneal surfaces and the pelvic/ paraortic lymph nodes for any metastatic foci of the disease.
- If there is free peritoneal fluid, it is collected in order to investigate whether it contains cancer cells (cytological examination). Otherwise, the above test is performed in the peritoneal cavity. The presence of cancer cells in the peritoneal fluid does not change the stage of the disease, but in some cases may affect the type of treatment after surgery.
- The uterus and the cervix (total hysterectomy) should be removed as one, in order to avoid direct contact of the tumor with the peritoneal cavity. Surgical removal of the fallopian tubes and ovaries is usually necessary. In young women who wish to avoid premature menopause, the ovaries may be preserved if the disease is early-stage and has generally mild biological behavior.
What is the role of lymphadenectomy?
Since lymph node metastases are an important prognostic factor in endometrial cancer, the excision of lymph nodes for histological examination can provide significant information for predicting the course of the disease and determining the adjuvant therapy. Depending on the histological type and grade of the tumor, imaging and intraoperative findings, removal of pelvic (common, internal and external iliac and thyroid lymph nodes) and, sometimes, paraortic lymph nodes (up to the level of the kidneys) may be required.
If there are swollen lymph nodes in the scan images or intraoperatively, their excision is necessary. Finally, if the disease appears to be confined to the uterus and does not have aggressive histological features, the investigation of lymph node metastases with the sentinel node biopsy contributes to their diagnosis, significantly reducing the complications of complete lymph node dissection (e.g. lymphedema, lymphocysts).
When should we perform an omentectomy?
Some histological types (e.g., serous, clear cell, carcinosarcoma) also require the removal of the omentum, a fold of peritoneum that connects the stomach to the transverse part of the colon (large intestine) and hangs down from it. In this context, omentectomy is usually supracolic.
How is surgery performed on patients with endometrial cancer?
Surgery in patients with endometrial cancer can be performed openly or with minimally invasive surgery techniques (laparoscopy, robotic surgery). The choice of techniques depends on the patient’s history, the preoperative characteristics of the disease and the experience of the Gynecologic Oncologist in the techniques. It is widely accepted, however, that when the disease appears to be confined to the uterus, robotic surgery and laparoscopy are associated with a reduced risk of wound infection, bleeding, thromboembolic events and length of hospital stay compared to open surgery. In fact, given that the oncological results remain the same, robotic surgery and laparoscopy are considered the preferred options by the respective scientific companies abroad (ESGO, NCCN).
How can I investigate the possibility of having hereditary endometrial cancer on histological examination?
MSI testing or tumor immunohistochemistry for MLH1, MSH2, MSH6 and PMS2 proteins is a necessary step in the modern treatment of endometrial cancer. Insufficient expression of these proteins may entail an inherited form of endometrial cancer (Lynch syndrome), which requires a corresponding genetic test of the patient with a blood test. Even if this is negative (non-inherited form of endometrial cancer), knowledge of microsatellite instability (MSI) or under-expression of the above proteins makes the patient, under certain conditions, a candidate for immunotherapy, if at some point she relapses.
Is there an alternative treatment if the patient cannot be operated?
In case of very elderly patients or women with serious health problems that greatly increase the risks of surgery, radiotherapy is the preferred treatment.
Adjuvant therapy
What additional treatments may the patient need?
Depending on the stage of the disease, the differentiation grade and the histological type of the tumor, endometrial cancer is characterized by a different probability of recurrence (low, intermediate, high). The above data, in combination with other factors (e.g., lymphovascular invasion, patient’s age, peritoneal fluid cytology results), determine the type of adjuvant therapy that the patient may need after surgery. The respective decisions must be taken in an Oncology Council, with the participation of a Gynecologist Oncologist, a Pathologist Oncologist, a Radiotherapist and an Internist. In cases where additional treatment is needed, the options are:
- Intravaginal radiotherapy (brachytherapy), which should be ideally administered at 6-8 weeks after surgery (the corresponding period should not exceed 12 weeks)
- External radiotherapy with or without intravaginal radiotherapy
- Chemotherapy of usually 6 cycles of carboplatin/paclitaxel
What are the main side effects of radiotherapy and chemotherapy?
Radiotherapy may cause urinary disorders (e.g., frequent urination, pain when urinating), bowel disorders (e.g., diarrhea), fatigue and changes in the vagina (e.g., shortening, narrowing, dryness) in some patients. Some of these go away at the end of the treatment, while others may persist for a longer period. On the other hand, chemotherapy is sometimes accompanied by fatigue, hair loss, nausea, vomiting, diarrhea, a drop in blood cell count or numbness in the arms and legs.
How does endometrial cancer treatment affect the patient’s sex life?
Ovarian removal in premenopausal women and, most importantly, radiotherapy can lead to vaginal changes that affect the quality of sex life. These can be treated by using vaginal gels with lubricating and moisturizing effect, as well as vaginal dilators. Sex counseling can also be very helpful.
What includes follow-up care upon completion of treatment?
Follow-up care after treatment is based on:
- Periodic clinical examination, including gynecological examination.
- Screening tests. The available options include computed tomography or magnetic resonance imaging and PET/CT, so the relevant decisions are made based on the doctor’s judgment and the symptoms that the patient may have.
- Tumor markers (CA-125) in blood, in the few cases that are elevated when the disease is diagnosed.